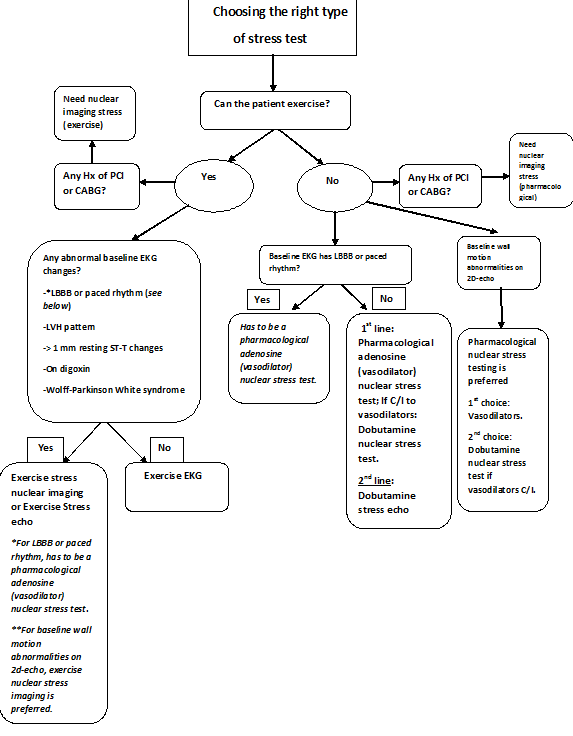
If you are like me, you always get a little flustered when you see many options on deciding what kind of stress test to order in your patient suspicious of CAD. This article will break down the main differences between different types of stress tests and provide you an algorithm next time you are faced with this quandary. So let’s begin:
The two main types of stress tests are exercise and pharmacological. Let’s just start with that and forget about imaging for now. So what kind of patient would be a candidate for an exercise treadmill test? It’s a patient that can walk at a hefty pace and well, exercise up to a certain exertion point. By guidelines, it is a patient that can “walk for more than 5 minutes on a flat ground or up to 1 to 2 flights of stairs without needing to stop.”1 So, if our patient has osteoarthritis of the knees and can’t handle this level of exercise workload, he or she wouldn’t be a candidate for an exercise stress test. Naturally, the only remaining choice would be a pharmacological stress test. Sounds easy so far? Good, because we are about to dig deeper.
Now, let’s assume that your patient can exercise and so you should obtain a baseline EKG for that patient. Why? Because if patient has an abnormal baseline EKG, we will need imaging to determine if any ischemic changes are present. Now, a bread-and-butter exercise EKG treadmill test is abnormal when you see a ST-depression > 1 mm in atleast 1 lead during the stress portion of it and within 7 minutes of recovery. That’s all you need: 1 lead! Also, the lead to keep an eye on is V5 which is the most specific and most sensitive.
Quick question: Does ST-depression during exercise EKG treadmill test localize ischemia to a particular coronary artery or region of the heart? No! However, in the instance that you see ST-elevation in leadswithout prior Q waves present there, that ST-elevation can localize ischemia to that specific region/coronary artery. ST-elevation in areas with prior Q waves does not indicate active ischemia but demonstrates further dysfunction of the infarcted myocardium and as you can imagine, worse prognosis.
Okay so having said that, if a baseline EKG already has any ST depression > 1 mm, then it wouldn’t be helpful to do an exercise EKG stress test on this patient as we will now need imaging. Other baseline EKG abnormalities for which exercise EKG treadmill test is not recommended are LBBB, paced rhythm, nonspecific intraventricular conduction delay > 120 ms, LVH, patient on digoxin, or pts with Wolff-Parkinson-White syndrome (WPW).
So now if your patient can exercise but has one of these aforementioned EKG abnormalities, what are our options? We have to use an imaging modality and it can be either stress echo or nuclear stress test (using technetium or thallium nuclear agents). What are technetium or thallium nuclear agents? They are radioisotopes which “light up” the heart to show the regions of activity and more importantly, inactivity with capture by gamma camera or through SPECT (single-photon emission computed tomography) technology during exercise. For these nuclear type of stress tests, which again can be pharmacological or exercise (we are currently focusing on the exercise aspect), there are two portions which make it a practical test. There is a resting portion where the images are taken during the rest and then during the exercise portion, when patient is put on a treadmill, 2nd set of images are captured. Naturally, these images are compared side-by-side to see what areas of the heart demonstrate ischemia. Makes sense? Great!
Okay, so couple exceptions now (you knew it couldn’t be that easy). For LBBB or paced rhythm, the only appropriate stress test is an adenosine pharmacological nuclear stress test. But why? Because, exercise or dobutamine will lead to septal motion abnormalities and septal defects in the setting of LBBB and can be interpreted as a positive stress test when that is not the case (false-positive!). In an event adenosine nuclear stress test isn’t possible (because patient is actively wheezing and thereby, bronchospastic), we can resort to exercise stress echo or dobutamine stress echo (preferred over dobutamine nuclear testing). We have to interpret it cautiously and focus on septal thickening rather than septal excursion. Another important exception: Patients with prior history of CABG or PCI: we should get stress imaging rather than just stress EKG as we want a test with a better sensitivity to ensure that this patient with already pre-existing history of coronary artery disease doesn’t have any new lesions. This concept inherently makes sense as we want to use a stress test modality with relatively high specificity and sensitivity in these particular subset of patients.
*If patient is morbidly obese, best option is stress nuclear imaging with PET scan, which is not an available option at many facilities. Also, if need to assess the myocardial viability, then can do nuclear stress test with PET or cardiac MRI (again not the easiest option available).
Okay, time for an intermission. We covered the stress tests with exercise treadmill involvement. Now it is time to discuss pharmacological stress tests.
There are 2 types of pharmacological stress tests and you can guess them by now:
1) Vasodilator or Dobutamine nuclear stress test imaging
2) Dobutamine stress echo.
Okay, so the most common vasodilators you will see at your institution are: Adenosine [Adenoscan], Dipyridamole [Persantine], and Regadenoson [Lexiscan]. When are these vasodilators contraindicated? When patients are actively wheezing or have bronchospastic airways, hypotension (in which case stress test should be cancelled altogether), or SSS or high-degree AV block (please don’t do a stress test under these circumstances). Another point to keep in mind: Withhold Theophylline 48 hours before this type of stress test and caffeine 12 hours before it as these drugs interfere with the efficacy of vasodilators.
Dobutamine is a sympathomimetic, which stimulates the beta-1 receptors and causes increase of heart rate (chronotropic effect) and increase in myocardial contractility (inotropic effect). Dobutamine is the stress agent used for pharmacological stress echocardiography as remember these patients are not stressing themselves on their own by exercising. It is also a 2nd-line agent for nuclear stress test in the instance when vasodilators are contraindicated. Why is it a 2nd-line agent? Because vasodilators cause great filling of coronary arteries compared to dobutamine and in an instance when vasodilators are contraindicated, atropine is commonly employed with dobutamine to achieve maximal coronary vasodilation. When should you not use dobutamine? You guys guessed it: Uncontrolled arrhythmias (A.fib with RVR, V-tach, etc) is the main contraindication. Other ones are when patient has HTN urgency, unstable angina, aortic dissection, and recent MI but remember all these reasons in themselves are reasons not to do a stress test in first place. One point to keep in mind when using dobutamine is to make sure that patient hasn’t taken his beta-blocker 24 hours prior to the stress test as patient may not achieve the satisfactory heart rate for successful validity of the stress test. Okay, so we covered all the salient points and I have designed the algorithm below to simplify your clinical decision-making. If you like the way this concept was explained, please let me know and I will do other topics. As always, use your clinical judgment in actual circumstances.
References:
- Askew, J.W; Chareonthaitawee, P; Arruda-Olson, AM. Selecting the optimal cardiac stress test. In: UpToDate, Post TW (Ed), UptoDate, Waltham, MA.
- Hanna, Elias. (2009) Cardiology-Handbook for Clinicians. Arlington, VA: Scrub Hill Press, Inc.