Patient presents to the emergency department with a complaint of “I can’t swallow.”
You as a physician are now assigned with a tall task of figuring out the correct diagnosis. There is always a temptation to gather the basic history, keep the patient NPO, and consult Gastroenterology to do an endoscopy.
However, that takes out the fun of being a super-doctor AKA the internist. An in-depth history-taking will help uncover the diagnosis long before the patient is on a table for an endoscopic procedure. So let’s begin:
First things first: #1 priority is to differentiate between oropharyngeal dysphagia and esophageal dysphagia.
Oropharyngeal dysphagia is defined as a disorder of the mouth and pharynx and patients usually have trouble STARTING the process of swallowing.
What makes up the oral cavity? Let’s see- there is the tongue, floor of the mouth, palate (roof of the mouth), and the tonsils. Go little further down and you encounter the base of the tongue, pharynx, larynx, and the cricopharyngeal muscles.
The symptoms of oropharyngeal dysphagia are manifested by:
-Food sticking in the throat, hoarseness, cough, pain in the throat, and referred pain to the ear
There is also drooling or spillage of the food and dysphonia (difficulty speaking). Clinical pearl: If you see tongue fasciculations, you should have strong suspicion for ALS.
How do we approach oropharyngeal dysphagia? Let’s focus on 3 broad categories:
1) Infection/inflammation 2) Structural 3) Neuromuscular.
In terms of infection/inflammation, one etiology which stands out is acute pharyngitis which can be bacterial (Group A Streptococcoal) or viral (more self-limited course). Candidiasis can also affect the oropharyngeal region in the form of thrush (suspect it in an immunocompromised patient).
For structural, Zenker’s diverticulum is an outpouching of the mucosa and submucosa above the cricopharyngeal muscle with a peculiar symptom of halitosis. What’s the best diagnostic test for it? Barium swallow! Don’t pick EGD- the answer is Barium swallow. Another structural pathology is oral cavity tumors which occur in patients with a history of smoking or alcohol use. In nonsmokers, think of HPV-induced squamous cell carcinomas.
For the neuromuscular causes, the etiologies of stroke, Parkinson’s disease, multiple sclerosis, myasthenia gravis, and ALS are the most common causes as identified by patient’s history.
Esophageal pathologies present with a sensation of food sticking in the lower aspect of the neck or the chest with regurgitation of food, chest pain, or heartburn. Patients will usually try to relieve the obstruction by sipping a glass of water.
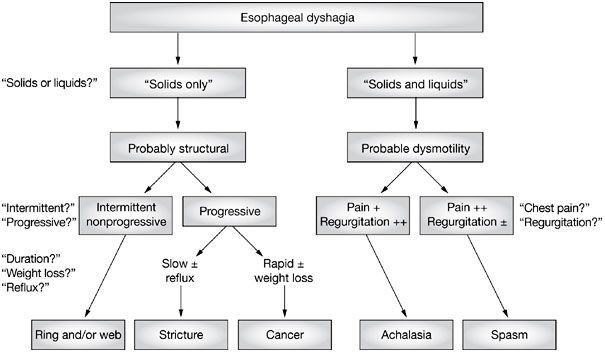
There is an easy way to approach esophageal dysphagia. Let’s divide into solids only and solid/liquids dysphagia. If a person has solid dysphagia, it is most likely a structural problem. What does that mean? It means that there is an obstructive process going on in the esophagus which is blocking the path of food to go down to the stomach. Sounds simplistic? It’s clearly not. Just look at the some of the etiologies of solid food dysphagia:
-Strictures
-Cancers (both squamous-cell and adenocarcinoma)
-Esophageal rings even the fancy one called Schatzki ring (A Schatzki ring– a narrowing of the lower esophagus by a ring of mucosal tissue).
Now let’s compare solid food dysphagia to solids/liquids dysphagia. This combined form of dysphagia tells you that it just can’t be a structural issue. Why can’t it only be a structural issue? Because liquids such as water don’t get blocked but can flow around the obstruction. But, if the esophagus has a motility issue such as diffuse spasm OR achalasia which is defined as the impaired relaxation of the lower esophageal sphincter with the absence of peristalsis, then liquids and solids won’t pass through. Achalasia on barium swallow is seen as “bird’s beak.” Of note, there is a term called pseudoachalasia which is often caused by malignancy (often submucosal gastric cancer) and its’ invasion into the lower esophagus.
Time to dig deeper: In solid food dysphagia, there is intermittent form and progressive form.
Rapid progression: Suspect malignancy and look for weight loss.
Slow progression with reflux-like symptoms: Think of a stricture.
Non-progressive and going on since childhood with an association of allergies: Bet on eosinophilic esophagitis being your top differential.
Side area of curiosity: What is an esophageal web? It is a thin piece of normal esophageal tissue consisting of mucosa and submucosa that can partially protrude/obstruct the esophagus. They can be congenital or acquired as a result of GERD. What do you call esophageal web + iron deficiency anemia? Plummer-Vinson syndrome. Webs cause intermittent non-progressive solid food dysphagia.
If solid/liquid dysphagia is associated with chest pain greater than regurgitation, you have to think of diffuse esophageal spasm also known as the nutcracker esophagus. Always rule out a cardiac cause first when working up this kind of chest pain. However, if regurgitation is the predominant symptom instead of chest pain in a setting of solid/liquid dysphagia, you have to ponder the diagnosis of achalasia.
Everything I just explained for esophageal dysphagia can be seen visually through this wonderful algorithm:
References: Epocrates
Dysphagia and odynophagia. In Gastroenterology and Hepatology: A Clinical Handbook, 15–26 (Eds Talley NJ et al.) Sydney: Churchill Livingstone.





